Pay, performance and the NHS
What can we do about the NHS – the UK’s National Health Service? Costs are spiralling, its IT failures are internationally infamous, and after several horrendous scandals, morale is at an all-time low.
The British government knows exactly what to do about it. It wants to pull back to a well-tried favourite: increase the managers, to give better control; tighten up the controls on targets and reporting; and back it all up with ‘performance-based pay’ – preceded, of course, by cutting the real-wages of front-line staff.
Yep: real innovation there…
Unfortunately, the one thing we know about all of these ‘recommendations’ is that every one of them will guarantee further failure: each has long since been proven to be a key cause of the problems complained about. I won’t give detailed references here – this is a blog, not a scientific journal, so I’ll assume that if you’re actually interested, you’re more than capable of looking them up for yourself – but just to give some examples:
— Managerialism and the quest for ‘control’: Directly linked to huge increase in costs, huge increases in paperwork, and systematic distraction from the actual purpose of delivery of healthcare. To give just one anecdotal example, when my parents were GPs (family-doctors) back in the 1970s, they had just two part-time clerical staff (in a country practice with three GPs) to cope with the inevitable paperwork. Since the 1980s, the paperwork has increased and increased and increased, such that in the late-1990s they had to add a whole extra floor to the surgery just to accommodate the number of paper-pushers: the total number of administrative staff (thirteen full-timers, last I heard) has roughly doubled with each passing decade. The vast majority of that paperwork is solely for keeping track of NHS ‘targets’; almost none delivers any clinical benefit. And there are still only three doctors in the practice, covering a hugely increased population and workload.
— Targets and reporting: Managers’ obsessions with ‘achieving targets’ have been directly linked to systemic failures, almost across the board: for example, the report on the Mid-Staffordshire scandal indicated that targets would invariably be ‘gamed’ – but especially so wherever financial-targets were linked to managers’ own ‘performance-based pay’. The blunt fact is that, in a health context (and arguably almost any context), targets simply do not work. What’s needed instead – as Simon Guilfoyle has explained so well for the police context – are metrics that actually mean something, and that can be used to guide context-appropriate decision-making.
— ‘Pay for performance’: Directly linked to demoralisation, dysfunctional behaviours and decreased performance – especially if, as is too often the case, the ‘performance-bonus’ goes only to the manager, and not his/her ‘reports’. The question of who defines what ‘performance’ is, and for whose benefit, is central, yet rarely addressed. Also, research such as that described in Dan Pink’s book Drive has long since proven that for knowledge-work and many (maybe even all?) other forms of applied skills, an inverse relationship is likely to exist between excess monetary payment (above a certain base-level) and actual performance – in other words, the wrong kind of ‘payment’ actually damages performance.
(Note, though, that crucial phrasing in the item above, about “above a certain base-level”. More money does not improve performance, but taking money away – as in the government is expressly aiming to do – brings the focus again on money rather than the overall desired outcome. For example, when pensions are linked to final pay, which is itself reducing in real terms, there are strong incentives to stop working, rather than continue to do the work – leading to serious loss of skills and experience in the workplace. It also reinforces the delusion that money is the only factor at play – which it most certainly is not.)
In short, not a good idea… none of it…
Reality, of course, is that the delusions of Taylorist managerialism are so deeply entrenched in government cultures that it’s unlikely – even at this dire stage – that the penny will finally drop. Oh well…
But just imagine – imagine – that we actually had a chance to tackle this properly, architecturally speaking, from a true whole-of-enterprise perspective: what would you do then? How would you tackle it?
Here’s what I would do:
— Start from purpose: Go back to the beginning: the original aim of the NHS was “health for all, free at the point of delivery”. Three key points arise from this:
- It’s about protection of health – a positive state – rather than treatment of disease – a negative state arising from lack or loss of health. This suggests that the focus should always be more on prevention than ‘cure’ – which is immediately problematic, because it’s difficult to prove or measure health in any absolute terms, and doctors and many others have a strong vested-interest in keeping the focus more on ‘cure’.
- It’s for all – including those with ‘pre-existing medical conditions’ and suchlike. This means that there will always be those who use the system more than others, or less than others – potentially creating social and/or political tensions that could well undermine the principle of ‘for all’.
- It’s free at the point of delivery – in part to reduce any additional stress for the patient under the sometimes literally-traumatic conditions occurring around the point of delivery. However, ‘free at the point of delivery’ is not the same as ‘free’: in a money-based possession-economy, it still has to be paid for somehow – which again can leave it open to sociopolitical challenge.
Subject to those provisos, though, a whole-of-enterprise architecture would and should use that initial purpose-statement as its touchstone in all decision-making.
(Since it should be clear, from even the briefest analysis, that we’re now a long way separated from that core principle – more usually supplanted by managerialism’s obsessions with ‘efficiency’ and suchlike – there is then also a significant architecture-challenge about how to move from ‘as-is’ towards a ‘to-be’ that matches back to the original ‘as-was’…)
— Acknowledge the nature of the work: In particular, explicitly acknowledge that much of the work has high levels of inherent-uniqueness, and outcomes that are often inherently uncertain. The first – and essential – understanding that should arise from this is that Taylorist-style management-methods based on sameness and ‘control’ are not appropriate to much if not most of this context, and should not be used.
(If command-and-control management-methods are used in this type of context, the inevitable outcome is an over-focus on pseudo-‘efficiency’ at huge cost to overall effectiveness, and huge levels of ‘failure-demand‘ – as is evidenced at present through almost all areas of the NHS.)
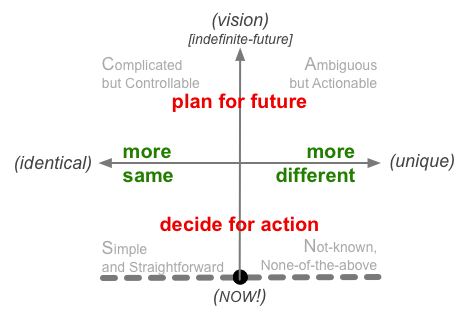
To summarise this visually in terms of the SCAN framework:
Taylorist concepts only make sense at the upper far-left edge of the frame: high-sameness, driven by abstract assumptions and assertions a long way distant from the ‘Now!’ of action. By contrast, much of medicine occurs in contexts described at the diametrically-opposite side of the frame, right down in the far corner of the lower-right: high-uniqueness, much of it changing in or close to real-time. For example, a recent article in the BMJ, ‘Military rather than civil aviation holds the answers for safer healthcare‘ [behind the BMJ’s paywall, unfortunately], summarises the point well:
Medicine has adopted several safety principles from civil aviation with mixed success. Examples include regulatory processes such as accreditation and incident reporting and standardisation techniques such as checklists; the so called sterile cockpit, which forbids non-essential activity; and handover briefings. …
[Yet] Translating rigid civil aviation processes indiscriminately into hospitals is not always appropriate. A better industry to consider for healthcare functions that require flexibility and autonomy is not civil but military aviation. … Military aircrews understand the importance of managing risk because they have to keep working in worst case scenarios, just like doctors.
Uncertainty is the fundamental fact throughout medicine: not so much Occam’s Razor, from mainstream science – reduce to a single ‘root cause’ – as Hickam’s Dictum, that “patients can have as many diseases as they damn well pleases”. Hence, for example, there needs to be explicit acknowledgement, right from the start, that things can and do ‘go wrong’: the best we can ever achieve is ‘better’, not ‘certain’. This has huge implications for insurance, risk-management, politics, patient-responsibility, social-relations and much else besides.
This also means that organisational concepts based on assumed ‘sameness’ – such as applying commercial ‘market’-type models, or promoting commodity-type ‘patient choice’ – are fundamentally inappropriate to the health-context, no matter how popular they may be with certain economists and politicians. The health-profession is already struggling with the crippling effects of hyperspecialisation: demanding structures and incentives that would actively increase that tendency is all too literally insane.
— Rethink the organisation of the work: Again, a SCAN mapping would probably help a lot here, identifying where standardisation and suchlike can and cannot be used. I’d also suggest, strongly, that the differences between measures (which do work) and targets (which don’t) should be hammered home at every step of the way. See, for example, Simon Guilfoyle’s brilliantly-ironic post ‘On purpose‘ for a simple, practical (and bleakly-amusing!) way to do this, and why we need to challenge ‘the machine’:
Workers can become very adept at meeting the machine’s definition of ‘purpose’, whilst simultaneously failing to attain the real purpose, which has now been obfuscated (the [‘Purpose Obfuscation O-meter’] machine does what it says on the tin). Sometimes, the workers still manage to meet true purpose, but fail to achieve what the machine thinks is the system’s purpose. This causes them to get in trouble. It also means that managers have to initiate a lot of audit and inspection to ensure that the machine is satisfied. Unfortunately this costs a lot of time, money and effort. It also makes the workers and customers or service users feel fed up.
The common complaint of politicians is that the NHS costs too much. And yet, right there, is a key cause of increased costs over the past few decades: the fundamentally wrong-headed mechanisms put in place to try to ‘control’ those costs. To take that earlier example from above, the administrative staff-levels at my parents’ surgery have more than quadrupled over that time, at huge increase in cost, and with mostly negative impacts on clinical outcomes (because much more of doctors’ time is taken up with reporting-paperwork) – yet in reality, most of those staff are tied up with reporting against ‘targets’ that have, at best, precisely zero meaning. Stripping out that nonsense and replacing it with measures that do make sense and that can guide clinical decisions would enormously cut both complexity and cost at a single stroke. Again, Simon Guilfoyle makes the point well, in his post ‘The Perfect Target‘:
As the greatest opportunity for performance improvement lies within the system, this is where effort should be focused. The first step is to reduce waste. Waste is the activity within a system that does not provide value to the service user, such as unnecessary internal reporting requirements, or time spent reworking what wasn’t done properly in the first place. If waste can be reduced (or ideally, eliminated), this generates capacity that results in a more effective system and improved service delivery. These improvements outstrip anything that even the most ambitious numerical target could aspire to reach.
Notice that almost none of this changes the front-line work at all: just the ‘control’-mechanisms that get in the way of doing that work in the first place…
— Rebalance the responsibilities for the work: Given the nature of the work, the old medical hierarchies of consultants, housemen and nurses never made much sense – but adding an extra layer of management-hierarchy on top makes it worse, and then throwing the muddled mess of so-called ‘patient-choice’ into the mix makes it even worse again. As Gene Hughson put it in a comment here, in relation to another similarly-chaotic context:
The wonder is not that things don’t get done, but that sometimes, despite the odds, there’s an occasional success.
We could perhaps illustrate this best via one of the views in the Enterprise Canvas framework. In the Taylorist paradigm, the ‘owner’ defines the purpose, ‘management’ runs the show, and everyone else – including suppliers and customers – must do what they’re told. (Notice that in this paradigm, the values and drivers that actually underpin the overall shared-enterprise are all but forgotten.) For the NHS context, the ‘owners’ are the government of the day, and the ‘profit’, in their eyes, is essentially in terms of keeping monetary-costs to the barest minimum, but otherwise much the same principles apply:
To make it work, we need to flip the whole structure the other way up:
All of the roles still exist here (and perhaps a few other previously-unacknowledged ones as well), but their respective responsibilities, and the relationships between them, are significantly different, including:
- guidance is driven by the core values and purpose – not primarily by the monetary focus of ‘cutting costs’
- the focus is expressly held on service-delivery and the service-cycle (‘before’, ‘during’, ‘after’) – not the ‘past-first’ orientation of Taylorism
- the government is merely one amongst many groups of investor/beneficiaries
- the role of management is reframed as one of a set of supporting-services (primarily ‘value-governance’ and support for continuous-improvement) – not the sole driver of the whole show
- the classic medical-hierarchies are reframed in terms of ‘distance from the point of action’ (the interface between the service and its ‘customer’ or service-user) – which means explicit acknowledgement that nurses and janitors, for example, are every bit as important to the overall outcomes as are doctors and surgeons
All players in the shared-enterprise are responsible for reaching towards the aims of the enterprise. Each player should respect the limits of their knowledge and responsibilities: for example, managers can advise on cost-implications of clinical-decisions, but should not attempt to ‘control’ those decisions on grounds of cost. And ultimately, each person is personally-responsible for their own health – in other words, the health-system can help, but it cannot do it for them, and must not attempt or pretend to do so, either.
In addition to rebalancing the responsibilities, we also need to rebalance between the various perspectives. Each player tends to view their own perspective as ‘the only view’ (or ‘only valid view’): hence doctors obsess about clinical practice, and politicians obsess about money, sometimes without regard to anyone else. At the very least, we need a better balance between ‘inside-out’ (the view from the clinic or hospital) and ‘outside-in’ (the view from the patient’s perspective – or that of the patient’s family, for that matter). Tools such as customer-journey mapping can help a lot in this, but there’s much more that we need to do – hence the importance and value of a whole-of-enterprise approach to the overall enterprise-architecture.
— Rethink how to reward the work: The first point here is that so-called ‘performance-based pay’ simply does not work, for almost all of the work that takes place within the health-context. (Not just ‘does not work’, it actively makes things worse.) Instead, we need to base incentives on what is proven to help in knowledge-work:
- autonomy – freedom to make appropriate decisions within personal work
- mastery – continual development of personal competence and skill
- purpose – a personal sense of engagement in the work (individual-purpose), and often also that it is contributing in some way way to ‘that which is greater than self’ (collective-purpose)
- fairness – a sense of balance and mutual-respect across the social dimensions of the context
Unfortunately, every one of these themes is explicitly either forbidden or blocked within the status-hierarchies of Taylorism: in other words, there’s a serious paradigm-problem here…
We also need to reprise the point made earlier above, that whilst adding money doesn’t help, removing it makes things worse – in part because of that all-too-often-forgotten theme about fairness. To get the performance we need, we first need to pay people enough such that money is no longer a driving issue – which, for many if not most front-line staff in the NHS, urgently needs to be a lot more than they’re paid at present. There are some valid arguments to suggest that some levelling-down could reasonably be applied at the ‘top-end’ of the hierarchy – especially for managers’ pay – but the political ramifications are probably more trouble than they’re worth. Instead, a far safer source for the ‘extra’ money is simply to tidy up the Taylorist mess of failure-demand and dysfunctional non-‘controls’, as described earlier above: recovering even some of the money currently wasted on that mess would more than cover almost any politically-feasible pay-increase for front-line staff.
And yeah, plenty more that we could explore here, of course, but that’s probably more than enough for now? 🙂
What would your thoughts be, on how best to sort out the mess? Comments and suggestions, if you would? Over to you…


Great post Tom (and the fact that I was quoted shades my opinion not a whit 😉 ). Blindly following “targets” is a fools errand – no matter how much one might worship standardization, a metric like mortality rate means something vastly different when applied to a dentist vs an oncologist. A cynic might observe that relying on the numbers can be used to absolve the decision-maker from responsibility for thinking through their choices.
@Gene: “A cynic might observe that relying on the numbers can be used to absolve the decision-maker from responsibility for thinking through their choices.”
Painfully true in rather too many cases, I fear…